 Add My Company
Add My Company
Sign In
We analyse the pros and cons of sterilization methods, including sterile filtration, radiation, chemical, and heat.
The sterilisation of microbial life and biological material is a prerequisite of both experimental and environmental control in laboratories across myriad disciplines.
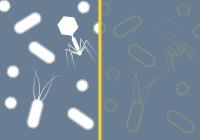
Whether ensuring aseptic conditions in a culture plate or maintaining an area of biocontainment, sterilisation’s goal is always the eradication of unwanted biological agents. This aim can be reached through a variety of procedural pathways, each with their own benefits and shortcomings.
The ideal sterilisation process needs to work quickly and effectively; deactivating microbiology and unwanted biological material such as prions. It should also ensure the minimal toxicity, health risks to operators, and change to sterilised objects, while providing maximum adaptability — accommodating different materials. The procedure should also be able to overcome any physical resistance to sterilisation that is demonstrated by the materials being sterilised. All of this should ideally be achieved in a cost-efficient way, which also allows for consistent monitoring [1] [2].
Meeting all of these conditions, however, is frequently impractical. Consequently, incorporating many of these factors is often a secondary concern based on situation and necessity, with the primary goal being achieving asepsis in a functional end product. What follows is an assessment of commonly available sterilisation methods, their positives, and negatives.
Sterile Filtration
If a fluid material is to be sterilised, filtration forms an option for consideration. A liquid or gas can be passed through a sterilising filter membrane, which forms a mechanical barrier to all particles of a larger diameter than the pores in the membrane. Microorganisms bigger than the pores are trapped behind the filter, assuring they cannot enter the filtrate.
Heat, radiation, and chemical sterilants work by changing the physical structures of molecules and organelle within microorganisms – a process which can also change the structural components of more sensitive substances. Filtration has no such effects, only removing particles over a certain size. As such, filtration forms a plausible choice more unstable and reactive fluids.
Unlike other sterilisation methods, filtration does not deactivate microbiological entities. As such, other sterilisation procedures - often heat or radiation - are required to sterilise the filter and residue post-processing.
Close attention must also be paid to the size of pores in the filter. Frequently, a pore size of 0.2μm is used — and with the smallest mycoplasma measuring around 0.3μm — this is sufficient for filtering out most bacteria. Yet ultramicobacteria can measure less than 0.1 μm [3] [4] [5], while viruses and prions are often smaller still. Reducing pore sizes to 0.001μm ensures fewer microbiological entities can enter the filtrate, although this becomes increasingly prohibitive to fluids that can be filtered. A decrease in pore size also increases processing time – a 0.1μm pore filter will have around 40% of the flow rate of a 0.2μm pore filter.
Radiation
As a sterilant, radiation takes multiple forms. Take, for example, ionising radiation sterilants; including x-rays, gamma rays, and electron beams. These technologies sterilise by electromagnetically exciting particles in the area being sterilised, causing them to release free radicals. These radicals combine with the double bonds in biomolecules, (such as DNA, RNA, and enzymes,) changing their form, stopping their function, and leading to the invalidity of the microorganisms containing them. Non-ionising radiation sterilants work by causing new bonds – pyrimidine dimers – to form between nucleobases in DNA, which – like with ionising radiation – changes the macromolecule’s structure and stops it functioning.
Due to their functionality, radiation sterilants can degrade organic chemicals such as plastics [6] [7] and biological material. Unfortunately, their degradative effects do not extend to prions which remain largely too stable to be affected by radiation sterilants. [8] However, it is worth noting that some studies show a possibility of prion denaturation via gamma radiation [9].
A further important consideration is that the penetrative ability and processing times of radiation sterilants vary significantly. Ultraviolet Light (UV) is only able to penetrate transparent materials, which makes it a viable sterilant for air and purified reverse osmosis water, but it is limited to a surface sterilant for opaque substances. UV’s processing time can also run into hours, as is the case with X-rays and gamma. However, these latter two methods bring their own advantages.
Gamma and X-rays are highly penetrative, meaning they can be used to sterilise objects held within otherwise impermeable containers. Electron beam sterilisation’s party piece is to sterilise near-instantaneously. Often it is used as a surface sterilant due to the electron particle’s poor penetrative abilities – however given enough energy it too can deeply permeate matter.
The running costs for X-ray, e-beam, and UV can be relatively low, with efficient electricity use an attribute of each. X-ray, e-beam, and gamma hardware have a high initial capital cost [10]. Gamma sterilisation has an ongoing cost associated with replacement of its radiation source, commonly the colbolt-60 isotope. It should, however, be recognised that while operators should always be shielded from the damaging effects of all radiation sterilants, the physical presence of radioactive material in gamma sterilisers mean extra precautions should be made during maintenance of the device.
Chemical
Chemical sterilants encapsulate a wide range of liquids and gases with one unifying feature – their ability to destroy microbial life. Due to these characteristics they are often harmful to humans, if not deadly. The most commonly used chemical sterilant – ethylene oxide – can cause headaches, nausea, vomiting, diarrhoea, shortness of breath, respiratory irritation, lung injury, and cyanosis in the short term, while long-term exposure is associated with occurrences of cancer, mutagenic changes, neurotoxicity, and sensitisation [11].
Ethylene oxide gas sterilises through the alkylation of proteins, DNA, and RNA, which causes microorganisms to be non-viable [7]. This process occurs as an effect of the high reactivity of the compound; an attribute which leads to logistical complications. Due to a combination of its toxicity and flammability, it is recommended that ethylene oxide is stored in a detached storage unit — with a 100m radius isolation zone established in case of a leak [12].
As with most chemical sterilants, Ethylene oxide is ineffective on prions and has the capacity to leave residue on sterilised surfaces. Its sterilisation time is also long – between 2 and 5 hours — and its processing time even longer; often at over 14 hours due to post-sterilisation vapour removal. Yet it is highly penetrative, works at low temperatures (between 29–65°C) and unreactive with most plastics.
One further interesting advancement in this area is gas plasma sterilisation. Hydrogen peroxide gas plasma is created by exciting hydrogen peroxide vapour using an electrical field, causing it to evolve free radicals that denature biological materials, as with the ionising radiation procedure. Hydrogen peroxide gas plasma has been shown effective against prions, works at low temperatures (37-44°C), and has a cycle time of less than 75 minutes, [13]. However the process has poor penetrative abilities and the hydrogen peroxide it relies on is a toxic, explosive substance.
Heat
Heat sterilisation is the oldest and simplest kind of sterilisation, and takes two forms – dry and steam. Key benefits of heat sterilisation include its ability to destroy all biological material (including prions), while leaving no contaminants or residue [14]. Another is the low cost, especially with regard to consumables: at most, only electricity and water are required. Hazards related to heat sterilisation are also low, although there is a risk of burns from touching hot sterilised objects.
Heat sterilisation effects the outer surfaces of the object being sterilised first, then spreads inwards until the entirety of a material has been sterilised. Heat denatures the proteins found in microorganisms and biological material, and as prions are proteins, they are also effected by heat sterilisation. The denaturing process alters hydrogen and disulphide bonds, and salt bridges, and alters the secondary, tertiary, and quaternary structure of proteins, rendering them invalid for biological processes [15].
Dry heat sterilisation involves creating an environment of 160°C to 170°C and maintaining it for between two and four hours. This combination of time and temperature mean sterilising heat sensitive material such as plastics via this method is unviable without material degradation [16], Blades have traditionally been sterilised with dry heat, as concerns exist over steam dulling them. However, studies have shown stainless steel blades sterilised with steam display negligible blunting [17].
Steam sterilisation is a faster and less heat-intensive process than dry heat sterilisation. Steam transfers heat energy more effectively than hot air which means a lower temperature (121°C – 134°C) and quantity of time (3 to 15 minutes) can be utilised for sterilisation. The boiling point of water at atmospheric pressure is 100°C, which is too low a temperature for the sterilisation process. As such, steam has to be generated in a pressurised atmosphere, which raises water’s boiling point to the required temperature.
Objects that can handle a heat of 134°C or less can be sterilised with steam, but must be able to withstand a combination of temperature, moisture and pressure. For those which can, steam sterilisation forms a highly effective and penetrative form of sterilisation.
Summary
The final conclusion for sterilisation isn’t straightforward. But it is possible to navigate through the complexities and find the right option by maintaining a key focus on the objects in question and their required condition post-sterilisation.
Filtration forms an excellent option for those sterilising a limited number of fluids – especially ones sensitive to heat, radiation, and chemical sterilisation. But decisions must be made in the knowledge that it is reliant on other forms of sterilisation to deactivate microorganisms from its mechanism.
Encapsulating multiple variants with different penetrative abilities, radiation is a good option if materials are heat sensitive and can withstand its damaging effects. However, it is expensive to set up and reliant on the scale of its use to be cost-effective.
Chemical sterilisation, while fraught with toxicity, residue, and logistical concerns, along with ongoing consumable costs, has its part to play when the object being sterilised is incompatible with other sterilisation techniques – for example a heat and radiation sensitive solid material.
For objects that are not heat, moisture, and — to some degree pressure — sensitive, steam sterilisation will often emerge as the standout choice; offering cost-efficiency, effectiveness, and speed. This is also the case for waste materials, where their post-sterilisation condition is not of concern. As such, an autoclave remains essential equipment for almost all laboratories, while steam-heated effluent decontamination systems (EDS) provide an excellent option for those with biologically active liquid waste to dispose of. Contact Astell Scientific via Info@Astell.com if you require more information about steam-based heat sterilisation.
Through analysis of the material being sterilised, it is possible to find a sterilisation technique that best fits the ideal model. A combination of speed, efficaciousness, materially compatibility, non-toxicity, adaptability, and ability to be monitored can all be assessed for the required situation, alongside the capacity to overcome any material resistance that may be found in the target material. Of course, cost-effectiveness will be a key factor in most organisations.
References
1. Schneider, P. (1994). Low-temperature sterilization alternatives in the 1990s. Tappi Journal;(United States), 77(1).
2. Rutala, William A., and David J. Weber. "Clinical effectiveness of low-temperature sterilization technologies." Infection Control & Hospital Epidemiology 19.10 (1998): 798-804.
3. Cavicchioli, Ricardo; Ostrowski, Martin (June 2003). Encyclopedia of Life Sciences. Nature Publishing Group. ISBN 9780470015902. Retrieved September 26, 2017.
4. Duda, V; Suzina, N; Polivtseva, V; Boronin, A (2012). "Ultramicrobacteria: Formation of the Concept and Contribution of Ultramicrobacteria to Biology". Microbiology. 81 (4): 379–390. doi:10.1134/s0026261712040054.
5. Janssen, Peter; Schuhmann, Alexandra; Mörschel, Erhard; Rainey, Frederick (April 1997). "Novel anaerobic ultramicrobacteria belonging to the verrucomicrobiales lineage of bacterial descent isolated by dilution culture from anoxic rice paddy soil". Applied and Environmental Microbiology. 63 (4): 1382–1388. PMC 168432.
6. Harrell CR, Djonov V, Fellabaum C, Volarevic V. Risks of Using Sterilization by Gamma Radiation: The Other Side of the Coin. Int J Med Sci. 2018;15(3):274-279. Published 2018 Jan 18. doi:10.7150/ijms.22644.
7. Qiu, Q.-Q & Sun, Wendell & Connor, J. (2011). Sterilization of Biomaterials of Synthetic and Biological Origin. Comprehensive Biomaterials. 4. 127-144. 10.1016/B978-0-08-055294-1.00248-8.
8. Rutala, W. A., Weber, D. J., & Society for Healthcare Epidemiology of America. (2010). Guideline for disinfection and sterilization of prion-contaminated medical instruments. Infect Control Hosp Epidemiol, 31(2), 107-17.
9. Gominet, M., Vadrot, C., Austruy, G., & Darbord, J. C. (2007). Inactivation of prion infectivity by ionizing rays. Radiation Physics and Chemistry, 76(11-12), 1760-1762.
10. Simmons, A. (2012). Future trends for the sterilisation of biomaterials and medical devices. In Sterilisation of Biomaterials and Medical Devices (pp. 310-320). Woodhead Publishing.
11. United States Department of Labor, 2020. Ethylene Oxide. [online] Occupational Safety and Health Adminitrator. Available at: [Accessed 25 September 2020].
12. National Center for Biotechnology Information (2020). PubChem Compound Summary for CID 6354, Ethylene oxide. Retrieved September 23, 2020 from https://pubchem.ncbi.nlm.nih.gov/compound/Ethylene-oxide. )
13. Cdc.gov (2020) Hydrogen Peroxide Gas Plasma | Disinfection & Sterilization Guidelines | Guidelines Library | Infection Control. Retrieved 27 September 2020, from https://www.cdc.gov/infectioncontrol/guidelines/disinfection/sterilization/hydrogen-peroxide-gas.html.
14. Rogers, W. J. (2012). Steam and dry heat sterilization of biomaterials and medical devices. In Sterilisation of Biomaterials and Medical Devices (pp. 20-55). Woodhead Publishing.
15. Mauer, L. (2003). PROTEIN| Heat Treatment for Food Proteins.
16. Vinny R. Sastri (2014). Material Requirements for Plastics Used in Medical Devices, in Plastics in Medical Devices (Second Edition).
17. Vendrell, R. J., Hayden, C. L., & Taloumis, L. J. (2002). Effect of steam versus dry-heat sterilization on the wear of orthodontic ligature-cutting pliers. American journal of orthodontics and dentofacial orthopedics, 121(5), 467-471.
First published in Labmate UK & Ireland, Volume 45, Issue 7.
For more information on ACHIEVING ASEPSIS - SELECTING A STERILISATION PROCEDURE. talk to Astell Scientific Ltd
Enquire Now
List your company on FindTheNeedle.

